Electroconvulsive Therapy, commonly known as ECT, is one of the most debated and misunderstood treatments in modern medicine. For many people, the very mention of ECT brings to mind dramatic movie scenes, old black-and-white hospitals, and frightening images of uncontrolled electricity. Yet behind these exaggerated ideas lies a treatment that has evolved over nearly a century, saving lives, reducing suffering, and helping patients when other treatments fail. To truly understand ECT, it is important to look at its beginnings, the controversies that shaped its reputation, and the ways it is used today in a safer, more scientific, and compassionate manner.
The Early History of ECT: Where It All Began
ECT was first introduced in the late 1930s by Italian psychiatrists Ugo Cerletti and Lucio Bini. At that time, mental health treatment was still developing, and doctors were desperately searching for effective ways to help people with severe psychiatric conditions such as major depression, schizophrenia, and mania. Cerletti and Bini observed that seizures induced in animals sometimes led to behavioral improvements. Based on this observation, they experimented with controlled electrical stimulation to trigger seizures in human patients.
Surprisingly, they found that many patients showed noticeable improvements in mood and thinking after treatment. In the decades that followed, ECT spread across Europe and the United States, quickly becoming one of the most widely used psychiatric treatments. However, the early version of ECT was crude by today’s standards. There was no anesthesia, no muscle relaxants, and very little patient comfort planning. This meant that although the therapy often worked, it also caused pain, injuries, and fear. These early practices would later fuel much of the controversy surrounding ECT.
Growing Popularity and the First Wave of Criticism
During the 1940s and 1950s, ECT became a common hospital treatment. Doctors valued it for one simple reason: it worked quickly and often dramatically. Patients who had been severely depressed or catatonic for months sometimes showed improvement after only a few sessions. Families saw loved ones regain their ability to speak, think, and function.
But alongside these successes came criticism. Some patients felt traumatized by the experience, while others reported long-term memory problems. Ethical standards in medicine were weaker at the time, and there were reports of treatment being given without full consent or understanding. Popular culture also began portraying ECT as harsh and inhumane. One of the most powerful examples was the film “One Flew Over the Cuckoo’s Nest,” which depicted ECT as a punishment rather than a medical therapy. This image deeply influenced public opinion.
Advances in Medicine: ECT Enters the Modern Era
By the 1960s and 1970s, medical science was rapidly evolving. The introduction of antidepressant and antipsychotic medications changed psychiatric treatment. At the same time, doctors and researchers began improving ECT techniques to make them safer and more humane. Today, ECT looks nothing like the earlier procedures that shaped its negative reputation.
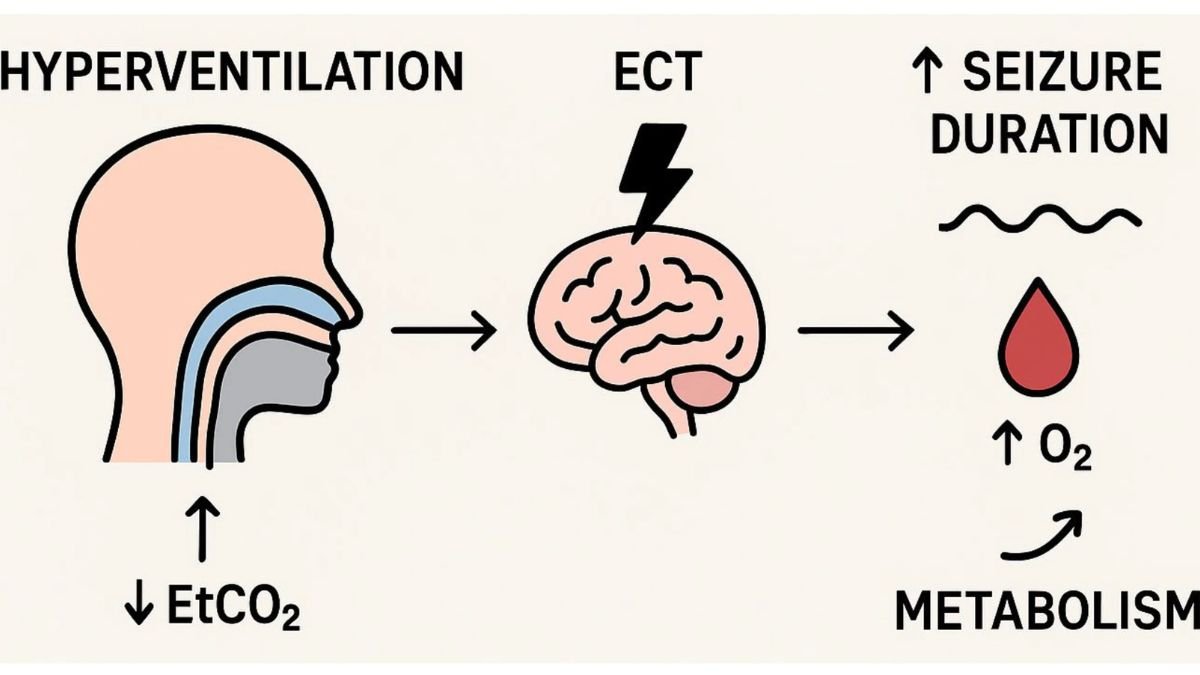
Modern ECT is performed under general anesthesia. Patients are asleep throughout the procedure and do not feel pain. A muscle relaxant is also given to minimize physical movement during the induced seizure. The electrical stimulation is carefully measured and targeted to specific areas of the brain, reducing unwanted side-effects. Treatment is provided by a trained medical team, including psychiatrists, anesthesiologists, and nurses, under strict safety standards.
The procedure itself usually lasts only a few minutes, while the patient spends about an hour in the treatment area for preparation and recovery. Most people receive a series of treatments over several weeks rather than a single session. Recovery is monitored closely, and patients typically return home the same day.
Who Receives ECT Today and Why?
In modern psychiatry, ECT is not used casually or as a first-line treatment. Instead, it is considered when patients have severe depression, bipolar disorder, schizophrenia, or catatonia that does not respond to medication or therapy. It is also recommended in situations where someone is at high risk of suicide or is unable to eat, drink, or function because of their mental health condition. In such cases, the speed of improvement can be lifesaving.
Many patients who undergo ECT have tried several medications without relief. Some experience severe side-effects from drugs and find ECT more tolerable. Research over the decades has shown that for certain forms of depression, ECT remains one of the most effective treatments available, with high response and remission rates. For people who feel trapped by their illness, ECT can offer hope and a path back to daily life.
Understanding the Risks and Side-Effects
Like any medical treatment, ECT is not without risks. The most commonly reported side-effects involve memory and concentration. Some patients experience temporary memory gaps, especially for events close to the time of treatment. Others may notice difficulty recalling past experiences from weeks or months before. In most cases, these memory problems improve over time, but in rare instances, some loss may be longer-lasting.
Short-term confusion and headache after treatment are also common but usually pass quickly. Because ECT requires anesthesia, doctors carefully evaluate each patient’s physical health before proceeding. Although complications are rare, the medical team remains prepared to respond to any issues.
These risks fuel ongoing debate about ECT’s role in psychiatry. Supporters highlight its effectiveness for severe, resistant depression and its ability to save lives. Critics argue that memory effects can be deeply distressing and that more research should continue into long-term outcomes. Both perspectives contribute to ongoing scientific discussion, pushing the field toward greater safety and understanding.
Ethics, Consent, and Patient Rights
One of the most important changes in modern ECT practice is the emphasis on informed consent. Today, patients must be fully informed about the benefits, risks, and alternatives before treatment begins. They have the right to ask questions, discuss concerns, and refuse therapy. In rare cases where a patient is unable to provide consent due to severe illness, legal and ethical safeguards are used to protect their rights and dignity.
This focus on respect and autonomy is a major reason why modern ECT differs so greatly from its early history. The goal is not only to treat illness but to ensure that treatment is compassionate, transparent, and patient-centered.
Public Perception: The Shadow of Old Misconceptions
Despite decades of improvement, ECT still faces stigma. Many people continue to associate it with outdated practices or frightening cultural portrayals. This misunderstanding sometimes prevents patients from considering a treatment that could truly help them.
Mental health professionals now work to educate the public, explaining that ECT is a medical procedure grounded in research, delivered under strict safety standards, and often life-changing for people with severe illness. Awareness efforts emphasize that depression and other mental disorders are real medical conditions, not signs of weakness, and that all effective treatments deserve fair consideration.
“What the Science Says About How ECT Works”
Scientists continue to study exactly how ECT improves mental health. While the full mechanism is still being explored, research suggests that the controlled seizure created by ECT leads to changes in brain chemistry and neural connections. These changes may reset or rebalance systems involved in mood and emotion. Brain imaging studies also show structural and functional changes after treatment, which may explain why patients often experience relief when other therapies fail.
The Future of ECT and New Alternatives
The future of ECT is closely linked to advances in brain science. New techniques, such as transcranial magnetic stimulation (TMS) and deep brain stimulation (DBS), are also being explored as alternatives or complements to ECT. These approaches aim to deliver targeted treatment with fewer side-effects. At the same time, refinements in ECT technology continue to improve precision and safety.
Rather than disappearing, ECT is evolving as part of a broader set of therapeutic tools. For some patients, it remains the most effective option. For others, new therapies may eventually take its place. What remains constant is the commitment to compassionate care and scientific progress.
Conclusion: A Balanced View of ECT
Electroconvulsive Therapy has traveled a long and complicated road, from its rough beginnings in the early 20th century to its refined, medically supervised form today. It has been praised as a lifesaving treatment and criticized as a source of risk and fear. The truth lies somewhere in between. ECT is neither a miracle cure nor a cruel relic. It is a powerful medical tool that must be used carefully, ethically, and with respect for every patient’s experience.
For people struggling with severe, treatment-resistant mental illness, ECT can open the door to recovery when hope feels distant. Understanding its history, controversies, and modern use allows us to see the therapy more clearly—not through the lens of stigma or myth, but through compassion, science, and human experience.